Trip Along The Prostate Cancer Highway©
by Tony Watton
Introduction
Right at the outset I need to emphasise that the following account is my own personal continuing adventure. The errors and omissions I have made in this and my approach to prostate cancer are all my own work. Every man's experience is an intensely personal one and each needs to discover the best way forward for himself, based on research, beliefs, expert advice and more than a little bit of luck (not necessarily in that order). Anyway, for what it's worth - here goes!
| Year of Cancer | Year and Event |
| 1 | 2004 - Diagnosis and High Dose Rate Brachytherapy Radiation |
| 2 | 2005 - In-dwelling Catheter |
| 3 | 2006 - Intermittent Self-Catheterisation |
| 4 | 2007 - Regular Visits to Peter MacCallum Clinic |
| 5 | 2008 - Radical Salvage Prostatectomy |
| 6 | 2009 - Suprapubic Catheter |
| 7 | 2010 - PSA Starts to Rise Again |
| 8 | 2011 - Blockages in the Suprapubic Catheter |
| 9 | 2012 - PSA Rises and More Bladder Stones |
| 10 | 2013 - Total Reverse Right Shoulder Replacement |
| 11 | 2014 - Bushwalking, Cycling and Bladder Spasms |
| 12 | 2015 - More Bladder Stones and PSA Increases |
| 13 | 2016 - Bike Ride Around Tasmania |
| 14 | 2017 - Riding the Munda Biddi Trail in WA |
| 15 | 2018 - Chemotherapy and Androgen Deprivation Therapy |
| 16 | 2019 - PSA Nearly Zero and Low Testosterone |
| 17 | 2020 - Abiraterone Commenced and Point-to-Pinnacle Walk |
| 18 | 2021 - PSA Undetectable and More Bike Rides |
| 19 | 2022 - PSA Still Undetectable and More Bike Rides and Walks |
| 20 | 2023 - Bike Rides, Catheter Leaks and a New SPC Site |
| 21 | 2024 - More Bike Rides, Walks and Rising PSA |
| 22 | 2025 - Bike Rides, Lack of Strength and Rising PSA, SAMRT Radiation |
2004 - Diagnosis and High Dose Rate Brachytherapy Radiation
History Before February 2004
I was born on 3/11/44, which made me 59+ years old in February 2004.
In common with many men nowadays, from September 2001 I had been having reasonably regular health check-ups that included blood tests and the occasional digital rectal examination (DRE) for any evidence of problems in that area.
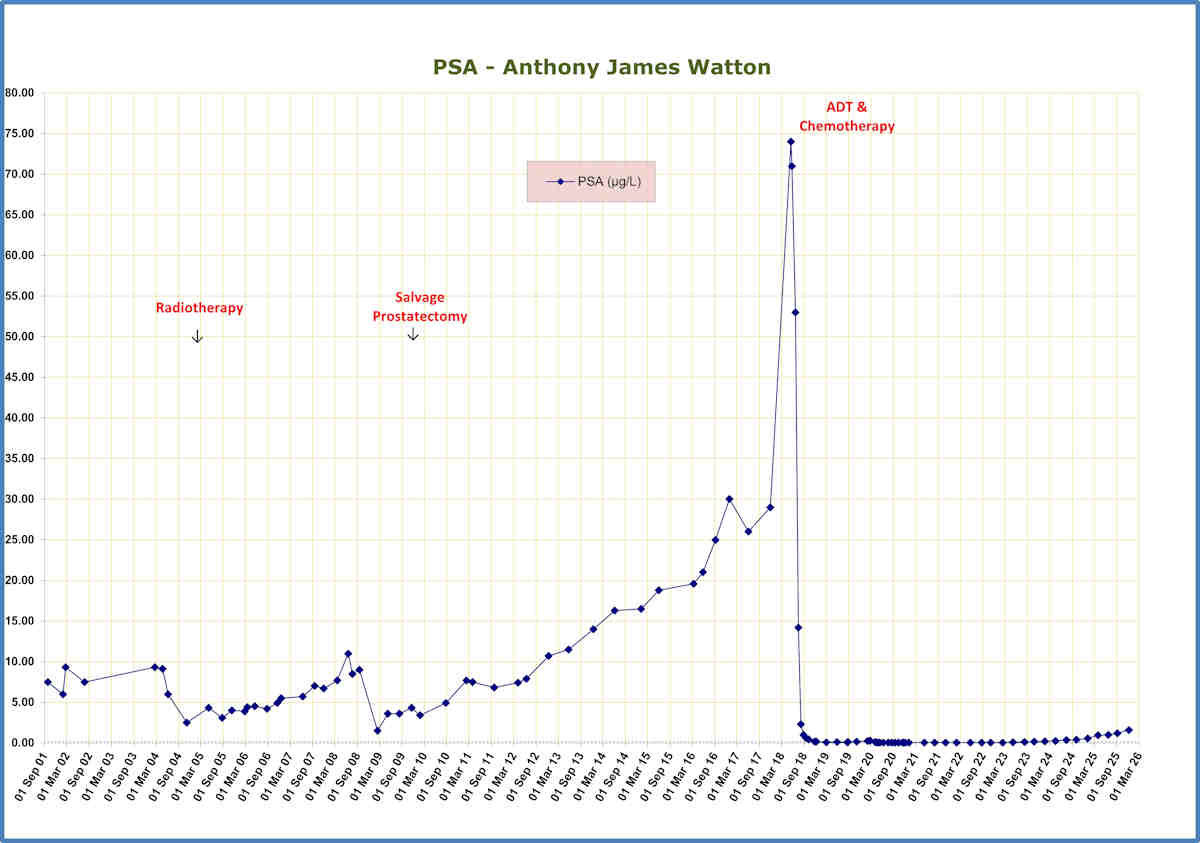
By the end of 2003 my GP was becoming concerned about the size of my prostate gland, which he detected was becoming enlarged and, I think, somewhat knobby. As can be seen from the PSA chart, my PSA was also at quite a high level (compared with the normal level of 4) at around 8. In retrospect, what was probably happening during this two-year period was what is called "watchful waiting". My personal view is that it does not appear to be very productive to be watching and waiting for things perhaps to get worse which, in my case, they certainly did!
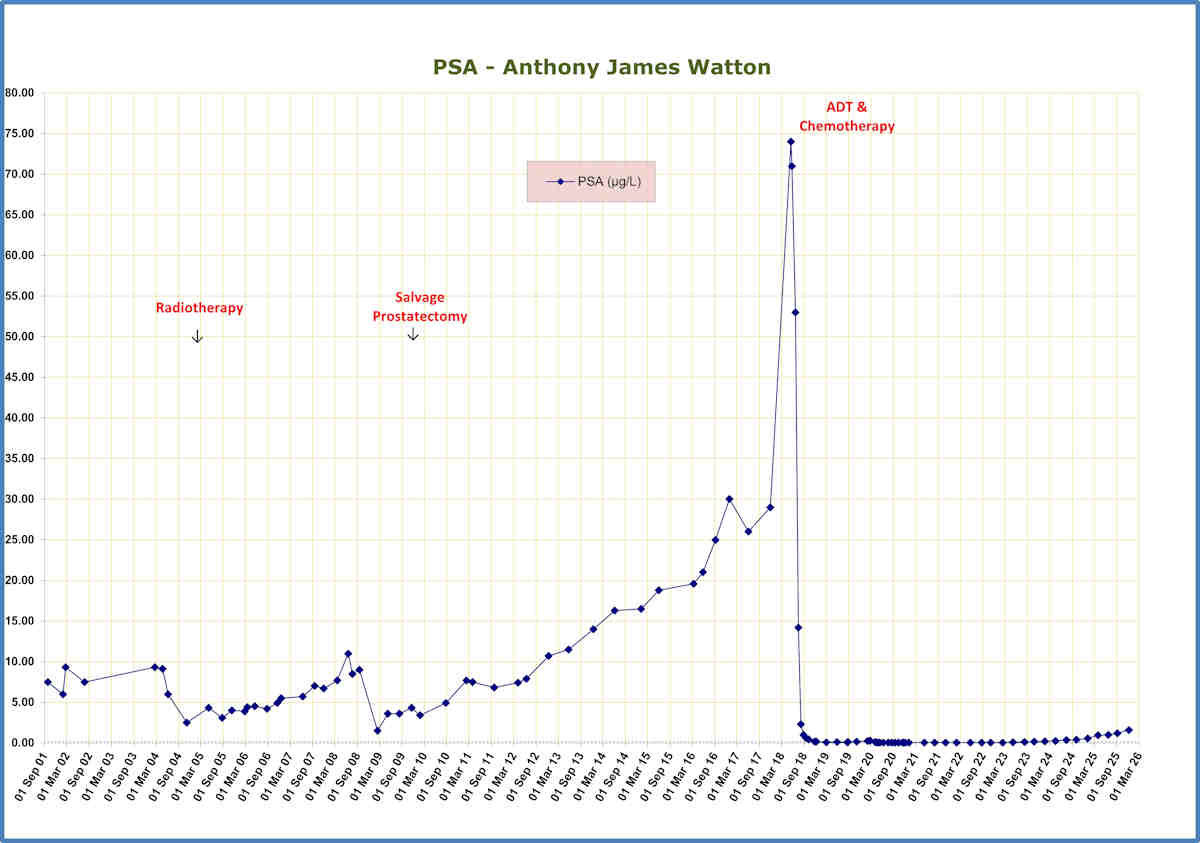
Updated PSA chart as at 15/12/25
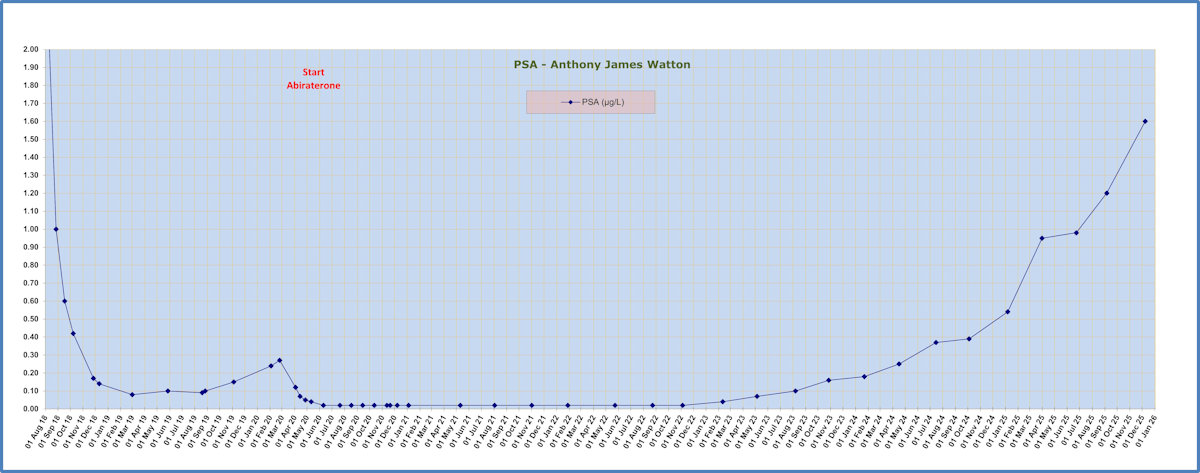
PSA chart since Chemotherapy and Hormone Therapy in July 2018
Having been booked in to see a local urologist in early February 2004, I had some prostate biopsy samples taken and then received the news that, "Well, you do have prostate cancer and here are your alternatives". I must admit I sat through that appointment in a bit of a fog, trying to absorb what I was being told but overwhelmed by the thoughts of what the consequences of the news might be.
The Gleason score for my cancer was 6, Stage 2 and the PSA at the time was 9.3.
My options for treatment were:
Watchful waiting (not preferred as mentioned above);
Radical prostatectomy (not keen on possible incontinence, impotence);
External beam radiotherapy (at the time a high risk of collateral damage to adjacent organs and relatively imprecise targeting so not preferred);
Low dose rate (LDR) brachytherapy with implanted radioactive seeds (worry about seed migration or poor location of the seeds, so not preferred);
High dose rate (HDR) brachytherapy with temporary implanted tubes for insertion and withdrawal of a radioactive source (fewest complications and/or side effects so my preferred option).
I was referred to an oncologist at the Peter MacCallum Cancer Centre in Melbourne for a further consultation as their reputation for treating prostate cancer was highly regarded.
Radiotherapy Treatment
At the consultation in Melbourne in March 2004 I was offered the opportunity to participate in a clinical trial to determine the effectiveness of HDR brachytherapy as a monotherapy. Details of this trial are at:
https://www.pubmed.ncbi.nlm.nih.gov/21550182
Normally, HDR brachytherapy is offered as a primary treatment to be followed up by external beam radiotherapy (EBR) a short time later. In view of my beliefs about the possible complications of EBR I was keen to be considered for the clinical trial and so opted for this course of action.
I was admitted
at
After
initial formalities, I
changed into
a
gown and
was
wheeled on
a
trolley
to the
operating theatre where I had
a spinal block administered to anaesthetise me from the waist down.
An
ultrasound probe was inserted into my rectum and this was used to guide the 15
straw length, 3mm (about) diameter hollow plastic “needles” that were inserted
into my perineum. These were held in place with a plastic template that was
sutured to my body with four sutures. A catheter was inserted into my bladder.
A large
triangular wedge was placed between my knees to prevent my legs closing. It was
also stressed to me that under no circumstances was I to move so that the
needles would touch the mattress. In other words, my pelvic area was motionless
on the bed.
Following
this procedure a CT scan was taken to make sure that the needles were placed in
the correct positions.
Then I was brought to the ward
to thaw out via the
Recovery Room where I found
three other patients.
I was hooked up to a saline drip (12 hours per bag) and PCA morphine (1 ml
per 1 cc). After the anaesthetic wore off I felt lower back
pain
and during the afternoon and evening used five doses of morphine. These were
automatically registered on the delivery pump equipment. I also had two Panadol
and vomited liquid, probably because of my empty stomach. I was given some
anti-nausea medication via the drip.
There was
frequent checking of blood pressure, pulse and O2 saturation level.
At about
There was a
dummy run during which each tube was checked for a clear run. A set of square
lead plates each 1m2 were then placed alongside my bed to shield the
radiotherapists, who were housed in an adjacent room.
The actual
treatment lasted about 15 minutes, with the pellet being inserted under computer
control into each tube in turn, for a predetermined time at different positions
within the prostate gland. The duration at each position depended on the
requirement for treatment at each location. A red light was on whenever the
pellet was out of its secure storage container.
After being
checked with a Geiger counter to ensure the pellet was not still in my body I
was then returned to the ward via the Recovery Room. I could only manage soup
for dinner, through a feeder with a straw, because I could only lift my head a
small amount.
My only
exercise was to gently raise my knees so that my feet were flat on the bed and
to bend my upper body from side to side. It was vital for me to keep my pelvic
area still as the needles protruded about 70 mm from my body and they were not
to touch the mattress, otherwise their positions in the prostate could have
changed. Consequently, I was on my back for a total of 56 hours from
Breakfast
on 12/5/04
consisted of two slices of
toast with jam, fruit juice and a cup of coffee.
Twice
during the day I was gently
rolled onto my side while my
back was washed and rubbed with Sorbolene to prevent stiffness and sores. This
was a welcome change from lying on my back inert, even though it lasted for only
a few minutes at a time.
Lunch was a
small pack of sandwiches and a cup of coffee.
At about
Dinner was
soup, ice cream, jelly and a cup of coffee. I deliberately refrained from eating
much because the last thing I wanted was to have a bowel movement while lying
flat on my back. My diet was deliberately set to be low residue meals. And it
wasn’t as though I was expending much energy anyway.
Once again,
sleep was difficult, with many interruptions. Eventually the night passed, with
the aid of a sleeping tablet.
The third day, 13/5/04
was uneventful, lying
on my back, talking to other patients, listening to my small radio and waiting
for
At
Along with
me also went the morphine that I was going to need prior to the removal of the
needles. The treatment lasted slightly longer this time because the radiation
source had decayed (half life of 74 days) over the three days of my treatment.
At the end
of this treatment I was advised to release a dose of morphine before the removal
of the needles. The doctor removed the four sutures holding the plastic plate in
place and then asked me to breathe in and out deeply three times and to hold my
breath on the 4th. As I reached the 3rd I felt a sudden tearing sensation as all
15 needles and the template were removed from my body. I think the ordeal would
have been worse if each of the needles had been removed separately. The catheter
was then removed and after a check that everything was OK I was wheeled back to
Recovery to wait to go back to the ward.
Once back
in the ward I sat
gingerly
on the edge of the bed before having a very welcome
shower and changing from the gown into pyjamas. It was a very pleasant feeling
to have the freedom to move as I wanted, with no restrictions. I had my first
solid meal in three days and enjoyed simply relaxing. I was given two laxative
tablets to assist with bowel movements.
I was released
from Peter MacCallum Clinic on
14/5/04 with
Ural to reduce acid in my urine and Voltaren to help the swelling to go down
where the needles had been.
I spent the
remainder of Friday then Saturday relaxing in a nearby hotel to get my body back to normal and
returned to Hobart by air on Sunday.
All this happened when I was still working as an accountant with the Natural Heritage Trust Unit of the Tasmanian Government, having taken two weeks sick leave for the purpose.
On returning to work in my three days per week part-time capacity I was able to cope reasonably well with the changes to my bowel and bladder habits that the radiotherapy had caused.
May 2004 to March 2006
During the time from 2004, as I was part of the clinical trial at Peter MacCallum Cancer Centre, I had my PSA checked each three months and made frequent trips to Melbourne for interviews and consultations with the oncologist who had treated me in May 2004.
As can be seen from my PSA chart, the level dropped to 2.5 in November 2004 and from that time started to climb somewhat erratically to about 4.4 by mid-March 2006.
The visits to Peter MacCallum Cancer Centre took on something of a ritual for me. I would catch a Thursday early flight (6 am) from Hobart; bus to Melbourne; walk to East Melbourne; cup of coffee and read the paper at Peter Mac cafeteria; appointment for 15 or 20 minutes with the oncologist; walk back to the Skybus terminal; bus to Tullamarine by 2pm and wait for the flight back to Hobart at 5.15pm. People would say to me, "Why don't you stay for a footy match or see the sights over a weekend?" but I wanted the visits always to be strictly single purpose with no distractions. A bit weird, eh?
All this time my urine flow rate was never really good but at the end of March 2006 my life changed direction again.
I was busy planting trees at our 4 ha Sandford property when I desperately needed to urinate. I hurried in to the toilet but, no matter how hard I tried nothing came. This was not a good sign. Acute urinary retention is the medical term. I phoned for an urgent appointment with my GP, was seen immediately and then referred to Calvary Hospital Accident and Emergency Department. I drove myself and the wait to be seen seemed to be interminable, desperately needing to urinate the whole time. The first doctor tried to insert a No 20 catheter to relieve my pain but failed. He then called for a urologist who managed to do the job.
The catheter was left in place and I was admitted for a cystoscopy and possible urethrotomy to clear the stricture. This was done the next day. When the catheter was removed in order to check my ability to urinate I was dismayed to discover that I still could not. The result was that I had another in-dwelling catheter (IDC) inserted and was sent home after another day with a leg bag, to be reviewed after one month.
2006 - Intermittent Self-Catheterisation
April 2006 to May 2008
At this next appointment the catheter was removed and I was instructed how to perform intermittent self-catheterisation. Initially this was to be a daily requirement, slowly becoming less frequent until after a few months I was using a catheter once a week to ensure the urethra was kept reasonably clear. This has worked quite well with only one or two occasions when I have had to revert to more frequent uses of the catheter.
My problem is that the urethral stricture is too close to the external urinary sphincter to be cut away without damaging the sphincter, thus causing more incontinence problems.
I left work at the beginning of April 2006 to concentrate on getting myself used to this new regime. I continued my PSA checks and visits to Melbourne during the remainder of 2006, through 2007 and 2008.
2007 - Regular Visits to Peter MacCallum Clinic
2008 - Radical Salvage Prostatectomy
In May 2008 the opportunity arose for me to see a visiting urologist from Sydney for a possible urethrotomy and dilatation of the urethra in an attempt to cure my problems without causing any additional ones.
However, the urologist was not prepared to cut away the stricture for the very same reason that it had not been done earlier. The result was that I was really no better off than I was before the procedure. The dilatation did not result in any appreciable easing of my urine flows.
June 2008 to January 2009
At about this time (June 2008) I started attending a local Prostate Cancer Support Group. It was interesting and enlightening to hear of other men's experiences and is something I intend to continue to do in future.
At one of my visits to Peter MacCallum Cancer Centre the oncologist expressed concern about my rising PSA which, by this time, had reached 11 (June 2008). He considered the distinct possibility that my radiotherapy treatment had failed to eliminate all cancer cells. Apparently, if a patient has three consecutive rises in PSA then it is assumed that the cancer is still present. This had occurred to me from August 2006 to June 2007 (4.2, 4.9, 5.5 and 5.7). On the other hand, there is a phenomenon called "PSA bounce" in which a man's PSA can rise temporarily for no apparent reason (usually within the first 12 to 18 months after radiotherapy) before settling down to a low level. I was hoping that was happening to me but realised the likelihood was that I still had cancer.
The oncologist wanted me to have a CT scan and a bone scan, but not before my PSA had reached a level of 15. This was because at a lower level (such as I was experiencing) the scans might be negative but the cancer was not sufficiently advanced to be detected. I was not happy with this scenario and asked to be referred to a Melbourne urologist for further advice. He also informed me that since 2004 there had been significant improvements in delivering the radiation compared with my treatment.
When the appointments were kept during July 2008 it was explained to me that, because I had already been exposed to HDR radiotherapy, no further radiation treatment could be given. Therefore, my options were: watchful waiting (again); hormonal therapy (not a cure but a delaying tactic); high intensity focused ultrasound (no Medicare assistance therefore $15,000 direct cost and still considered to be somewhat experimental); or salvage radical prostatectomy.
Salvage Radical Prostatectomy
Although I seriously considered hormonal therapy, my view was that if I opted for that course of action I may never have the opportunity for surgery at a later date if the cancer were to spread outside my prostate gland, whereas if I had surgery and it was not successful then I may still be able to have hormonal therapy later on.
Surgery appeared to me to be my best chance of curing me of cancer by physically removing the prostate and cancer cells. Whether it could be done or not depended on a biopsy being positive for cancer, CT and bone scans being negative and the prostate gland being relatively small (40cc or less I think).
My Hobart urologist informed me that nobody would undertake
the surgery in Tasmania owing to the high risk of failure and/or serious
complications;
i.e. death,
colostomy bag if the bowel were to be damaged, permanent incontinence, etc.
The biopsy was taken at the end of October 2008 and proved positive for 5% of one of the six samples taken. The scans were done and were negative and apparently my prostate was small enough for the operation to be considered. The urologist told me it was difficult to obtain the biopsy samples as my prostate was hard and somewhat shrunken (I imagine like a prune).
Therefore, on 2/12/08 the
salvage radical prostatectomy
operation was performed in
An issue that had been glossed over was that, because roughly 5cm of my urethra had been excised, (the urethra passing through the prostate gland) my penis had been reduced in length by that amount. However, the important factor was that an attempt had been made to cure me of prostate cancer. I have learned to live with an ornamental penis, although it would have been nice to have been offered an inserted graft to restore me to my pre-operation condition lengthwise!
I returned to
Problems
occurred almost immediately, however, when my urethra closed several times
during the following two days, stopping any urine flow except when I inserted a
No 16 catheter. Doing this caused quite a deal of pain when I pushed the
catheter into my urethra, without the benefit of any anaesthetic.
On 24/12/08 in desperation I phoned the two urologists with whom I have current referrals, only to be told they were closed until after Christmas. My local GP and the community nursing service both said they would not insert a catheter where a stricture existed so I arranged for a referral to Calvary Hospital Accident & Emergency and had a No 16 IDC inserted into my bladder.
The love, care and support I have received from both my wife, Suzanne, and my son, Matthew, have been of enormous benefit and comfort to me. Thank you to you both.
January 2009 to September 2009
Yes, the saga continues! At the urologist's appointment in January the IDC was removed and I was able to use a No 16 catheter every few days until my next appointment in hospital to have another urethral dilatation in an attempt to enlarge the urethral stricture.
At this time my PSA was tested again (1.5). My urologist said he would have liked the reading to be zero but I wasn't too disappointed at this level. However, it did mean that there were still cancer cells present.
Between February and August (my next urologist's appointment) I continued to self-catheterize every 2 or 3 days but the stricture was making this more and more difficult. I had to reduce the size of the catheter from a No 16 (about 6mm) to 10 (3mm) or 12 (4mm) by August. However, I felt I was coping, even though it seemed as if my waterworks were ruling my life most of the time.
Side Issue
Oh, I nearly forgot - in April I was on a short bush-walk on the Meehan Range (not a National Park) with my son and dog (Topsy). We were scrambling down a steep, loose gravel and rock fire trail when my right foot slipped from under me. I think my dog pulled me, rather than it being any fault whatsoever on my part!!
Anyway, my foot stopped against a rock but my body continued on past it. I heard a crack, squealed like a stuck pig and fell onto my back with my foot bent up under me. Matthew, who was following, said it looked horrible. When I regained my composure and got my foot out from under me I found I could still move my ankle, giving me some cause for optimism. I did not take off my boot. We thought about our situation and decided Matthew could walk over the ridge back to Mornington to get his car while I hobbled with Topsy along the 1km level fire trail to meet him at the end of Belbins Road. Not a pleasant trip (walk, stumble) but we got there eventually.
Back home and it was time to look at the damage. It did look horrible so Matthew took me to Calvary Hospital Accident and Emergency, where an x-ray confirmed what I had feared - the fibula was broken, but not displaced, near the lower end. This resulted in a polyurethane cast for eight weeks - no weight on the foot and an invalid once again. I must say Suzanne was wonderful during that time because I am not the ideal patient - rather an "impatient".
Now, in September, my right ankle is virtually back to normal. The swelling has reduced and I am anxious to get strength back into it to continue with my bush-walking plans. In late August as a trial Matthew and I walked from Cockle Creek to the coast and back as a test. A very enjoyable day out even though the weather was less than ideal.
Suprapubic Catheter
Back to the Main Event
At the August urologist's appointment he said the catheter situation was not satisfactory and things would not improve. He had previously talked to me about an SPC inserted directly into the lower abdomen and into the bladder, thus bypassing the urethra entirely. It did not appeal to me but I had to acknowledge the reality of my situation so I agreed to have the procedure.
The operation was to have been done on 1/9/09 but it was not proceeded with due to the possibility that my bladder had adhered to my colon and the fact that my bladder is smaller now, only holding a maximum of about 200mls, rather than the 500mls or 600mls in the past.
The procedure was re-scheduled for 10/9/09 when the SPC was inserted during open surgery. I am now recuperating from another operation and wondering if I will eventually have a valve fitted at the outlet to control urine flow or if I will continue to use a leg bag for the foreseeable future or maybe even go back to self-catheterization.
Update on my PSA - the May reading was 3.6, as was also the August reading. I suppose I am feeling relaxed about these results. At least it has not gone up recently! Also, I haven't yet reached high levels such that I will need hormonal therapy. I imagine that time will eventually come, however.
For what it is worth I have been drinking 300mls of pomegranate juice each day since January 2009 in the belief that it might delay the progress of my cancer.
Fingers crossed!
Update for December 2009
As can be seen from the PSA chart at the beginning of this account, my PSA has now risen to 4.3 - maybe not a dramatic increase, but nevertheless an increase. I am still taking 300mls of pomegranate juice daily; who knows if there is a beneficial effect or not as I do not have a "control group" against which to test myself. The urologist said, at the November appointment, that he expects the PSA level to rise but does not want to start me on hormonal therapy until the PSA reaches 10 or so. In the meantime, I try to get on with life and am not stressing about what my PSA may be at some time in the future.
A big test for me was how I was going to manage with a leg bag on my latest bushwalk with my son, Matthew. In the end I decided I could cope better with a self-made short tube with slide tap near the end to assist with urination now that my urethra is permanently blocked. My trip report is at Port Davey Track - December 2009 with a bit of detail as to how I coped on that 6-day walk.
Our next challenge will be a 10-day walk/climb from Cockle Creek to Precipitous Bluff (via New River Lagoon) and return during the 3rd and 4th weeks of January 2010. Matthew has already made this trip twice, on each occasion by sea kayak. His accounts of his trips are at Precipitous Bluff - Kayak and Walk - March 2005 and Precipitous Bluff - Kayak and Walk - January 2008.
I can't wait!
2010 - PSA Starts to Rise Again
Update for February 2010
Well, we did the Precipitous Bluff trip from 8 Jan to 17 Jan 2010 (10 days with a rest day in the middle). See my report at Precipitous Bluff from Cockle Creek - January 2010, with some comments about my catheter situation. This was a tremendous personal physical challenge and, thanks to Matthew's patience and tolerance, it was a memorable trip.
Since returning I have had a complete physical checkup, with all sorts of blood tests, including PSA. For some unknown reason my PSA is now 3.4 (25/1/10). I don't think there is any point in my trying to analyse the possible reasons - that's just what it is at the moment. However, I suppose I must be cautiously optimistic. It will be interesting to get the urologist's reaction at my next appointment towards the end of February 2010.
My next challenge will be to start using my Giant XTC2 mountain bike that I have set up as a touring bike with a BOB Yak trailer. I have plans to ride down to Cockle Creek before Winter sets in but much training to do before that happens.
Update for October 2010
Winter came. Winter went. Bike riding has taken a bit of a back seat in my list of activities recently as we moved house in July after putting the Sandford house on the market. It took seven months to sell and we are now back in Lauderdale, in the same street that we left six years ago to move to Sandford. Déjà vu all over again as they say in the classics!! We can see our old house 100 metres along the road.
At the appointment in late February the urologist was fairly happy with my progress, particularly how I was coping with the suprapubic catheter (SPC). It is now just another part of my life and has become a daily routine to take care of it. Every four weeks the catheter is changed by a nurse at the local Community Health Centre.
My next appointment is in August 2010, by which time I will have had another PSA test.
In June Matthew and I walked the Overland Track again, this time from south to north and from Lake St Clair. My report of the trip is at Overland Track South to North - June 2010.
As we used the huts on the trip it was a bit easier for me to look after my catheter. It meant that I did not need to crouch in a tent to change the dressing each day, as I did on our earlier south-west trips.
My PSA test result in August (please see chart at the start of this account) was 4.9. A bit disappointing as the February result was 3.4. Apparently, I have a permanent urinary tract infection (UTI) that in normal circumstances would be treated with an appropriate antibiotic. It is caused by the foreign body (catheter) being fixed in my bladder. Unless I develop a fever or other serious symptoms there is apparently little benefit in having any treatment because I could develop a resistance to the antibiotic that would render it less effective when it is really needed. The reason for mentioning the UTI is that it is possible that it has an effect (unknown) on the PSA result. Up or down, who knows?
The next appointment with the urologist is in February 2011.
Watch this space for developments.
2011 - Blockages in the Suprapubic Catheter
Update for February 2011
OK - first things first. PSA is now 7.7 and probably will continue to rise. When I received the results of this and other tests from Pathology my initial thoughts, when I opened the envelope in front of my wife and son, Matthew, were "Oh well, what did I really expect?" At least I am not experiencing any adverse physical consequences of still having prostate cancer. People put up with a lot worse, etc etc. [Updated chart is at the start of this account.]
Various comments I have read on the web indicate that having a UTI is likely to affect a PSA result (as mentioned above). The urologist, at the appointment today (17/2/11), has told me that it is very unlikely to have affected my result. However, he has agreed to put me on a course of antibiotics prior to having another PSA test in a few weeks time in order to put my mind at rest (or at least to eliminate the possibility of the link from my mind). I have decided to give up on the pomegranate juice - it was not a particularly pleasant drink anyway and, at $5.50 per litre every three days, was not a cheap drink. Apart from the disappointing PSA level I am coping reasonably well with the SPC - it's now just another part of my daily life and has not stopped me from doing everything I want to.
As far as bushwalking is concerned - a few weeks ago (mid-January 2011) Matthew and I walked from Waterfall Bay to Fortescue Bay. This was a longish day walk on a magical coastal walk - no bog to hinder us and a wonderful experience.
More recently - on Monday 14/2/11 in fact - we undertook a long day walk from Cockle Creek out to South-East Cape, the most southerly point in Australia that it is possible to walk to. An account is at Day Walk to South-East Cape, Tasmania - February 2011.
Plans for the near future and later include the Mount Anne Circuit, a visit to South-West Cape, another trip to Frenchmans Cap in the hope that we might get to see some views from the summit at last and others too numerous to think about. Also, I still have not ridden to Cockle Creek or around Tasmania in a single trip yet ......
Update to October 2011
After the course of antibiotics I had another PSA test on 31/3/11 - 7.5. I suppose this proves that the UTI is having a negligible effect on my PSA readings - it was worth finding out anyway.
Another memorable walk towards the end of February 2011 - to North-East Ridge near Mt Anne - a very tough walk on an overgrown track but worth every minute. Report of Matthew's and my walk is at Pandani Shelf via Sandfly Creek Track - February 2011.
Medically, things have not been too rosy during the past four months. As mentioned previously, my suprapubic catheter is changed every four weeks at the local Community Health Centre. There was a normal catheter change on 27/4/11 but at 2.30am on 12/5/11 I woke with the excruciating pain of needing to urinate but not being able to, as the catheter was blocked. In desperation I drove the 30-minutes trip to Calvary Accident and Emergency Department and eventually had the catheter changed by the on-duty doctor.
Things settled down for a while until, at 8am on 11/6/11 the same problem occurred again - needing to urinate but being unable to. Again I drove to Calvary and had the catheter changed. I was beginning to wonder just what was happening to me.
Within a week, at 12 noon on 18/6/11, the same problem arose again but this time I went along to the local doctors' surgery and was able to have the catheter changed there. On this occasion I asked if I could have the old catheter checked to see what might have been the cause of the blockage and was amazed to see the end of the catheter entirely blocked by a number of small stones of some sort. [Since then I have read about bladder stones but at that time I was ignorant of their existence.]
The next occasion (29/6/11) when I suspected that a blockage was occurring I arranged for an urgent catheter change at the Community Health Centre before my problem became serious. I brought the old catheter home and dissected it to find out what the cause might be. The following images show how large the stone was and that it almost completely blocked the end of the catheter.
By this time I began to believe that the stones were caused by the Calvid calcium supplement I had been taking on a daily basis to improve my bone density. I needed this because when I had had my bone density checked by x-ray about a year previously I was told that I had osteopenia (a precursor to osteoporosis). I stopped taking the Calvid.
Following these episodes I contacted the urologist who was handling my case and he booked me in for a day procedure of a bladder wash-out and possibly to insert a larger diameter catheter to help reduce the incidence of blockages. This occurred at the end of July 2011 when I was handed a plastic jar with the stones that had been extracted from my bladder. As I had mentioned to him just before the procedure that I was reluctant to have a larger catheter if it could be avoided he used the same size in the replacement catheter.
Life has now returned to "normal" - with no further blockages and back to four-weekly catheter changes. But, as I am no longer taking the Calvid (and my bone density had returned to normal) I wonder if my bone density might be suffering as a result. At present it is a small price to pay for the relative comfort of no bladder blockages.
My latest blood test for PSA (23/9/11) was 6.8. This was a bit of a surprise as I had prepared myself for a modest increase in the level (from 7.5 at last check) - to maybe 8 or 9 at least. So, what has caused the drop, I asked myself? The only sensible (?), logical (?) explanation is that my taking pomegranate capsules (2 x 500mg per day), combined with some exercise, has helped to keep my cancer under control. At the appointment with the Urologist on 3/10/11 he expressed some pleasure at the reduced result but offered no explanation. Next appointment in six months time.
During the early part of September Matthew and I undertook a 5-day walk on Maria Island (notes at Trip to Maria Island - September 2011 ).
Next venture might be my long-overdue and much anticipated bike trip down to Cockle Creek with Matthew over a six-day period at the end of October. In the meantime I must continue my bike riding to get some bike fitness back into my body. The only downside to bike riding is that the end of the catheter that's in my bladder causes some irritation and so there is blood in my urine for a day or so.
2012 - PSA Rises and More Bladder Stones
Update to April 2012
I must admit I was slightly disappointed that my PSA level was 7.4 at the latest blood test just prior to my appointment with the urologist in April 2012. However, on the bright side, it hadn't jumped up dramatically so no real cause for concern. Also, I have not experienced any more blocked catheter episodes and I am, therefore, convinced in my own mind that they were caused by my taking the calcium supplement, Calvid, and my body simply did not need the extra calcium.
Just to be on the safe side, I have been booked in for a June hospital appointment for another cystoscopy via the catheter site to make sure there are no stones lurking in my bladder. Apart from that, life goes on as "normal", meaning that I try to get on with things like bushwalking and bike riding whenever I can. In July I am scheduled to have another bone density test to check whether I am any closer to osteoporosis than I have been in the past.
The ride to Cockle Creek actually went ahead towards the end of October. It was a hell of a trip - report is at Ride to Cockle Creek. Also, one of my other "must-do" adventures was attempted, but not quite entirely a success - our walk out to South-West Cape ( Walk to South-West Cape ) in early March 2012. This has really only whetted our appetite for another trip in this remote area, mainly to do the South-West Circuit, including completing the walk out to the Cape as well. In the meantime I am planning more bike riding trips - the latest was a day ride to Dunalley ( Day Bike Ride to Dunalley ) with more to come as time permits. [I now do not understand how I found the time to hold down a full-time job with so much to do in retirement !!!]
Apart from the June 2012 appointment, I expect my next scheduled appointment with the urologist will be towards the end of the year, possibly early December. In the meantime, life goes on.
Update to June 2012
In two months my PSA has risen from 7.4 to 7.9. I realise I still have prostate cancer but that was a bit of a surprise. I am maintaining my dosage of pomegranate capsules each day - maybe they help and maybe they don't. Not having a control group makes it all a bit of a guessing game for me.
The cystoscopy and bladder wash-out that was performed on 19/6/12 resulted in there being a 1cm size bladder stone that, fortunately, was taken out. No idea why that grew but I suppose I can expect more in the future. On a positive note, the urologist is quite happy with my progress and does not consider it necessary for me to have another appointment until 12 months have elapsed, at which time I will have another bladder wash-out as a hospital day patient.
In the meantime, I am planning another extended solo cycling trip, taking everything with me, this time around the State in a clockwise direction. I am planning to leave in early November and expect the trip to take around a month to complete.
The next PSA blood test (and other blood tests) are due in early December 2012. It will be interesting to find out how things have changed.
Update to December 2012
Wow - that wasn't what I expected! PSA up from 7.9 to 10.7. Apart from that, I don't feel any different, which is some consolation at least. Apparently, when my PSA reaches about 15 I may need to commence hormonal therapy. From all accounts this will not be a particularly pleasant experience but I now have no reason to expect that that level will not be reached, maybe sooner than later.
The bike ride that I mentioned earlier actually eventuated but did not turn out exactly the way I had planned. Notes about the "trip" are at Bike Ride to Wayatinah.
In the meantime, life goes on as normal, with the next appointment with the urologist being the bladder wash-out in June 2013.
2013 - Total Reverse Right Shoulder Replacement
Update to June 2013
On 4/6/13 I had a hospital day procedure for a suprapubic cystoscopy and bladder wash-out. According to the urological surgeon there was some debris in the bladder that needed to be removed. During the past year I have had no problems with any blockages in my catheter so this was a precautionary operation rather than one designed to correct my situation.
My PSA has now reached 11.5. I know it won't go down but the surgeon told me that my cancer is not an aggressive one and it should be about two years before my PSA reaches a level of 20, which is the level he now wants to start hormonal therapy - not at 15 as I noted above. After that hormonal therapy should give me another three years. That's a target to beat if ever I saw one!!
Going back in time a bit - during March Matthew and I did a two-week bike riding tour of Flinders Island. This was my first visit to the Island but I hope it won't be my last. Notes about the trip are at Bicycle Tour of Flinders Island.
We now have plans to do a similar tour of King Island. Also, I still have plans to ride around the State, in an anti-clockwise direction, maybe towards the end of this year. Nothing definite yet though.
Update to December 2013
As shown in the chart at the beginning of this ramble, my PSA has now risen to 14.0 at the latest test in December. I know I am repeating myself, but on the bright side I still have no extra ill-effects of having cancer but I sometimes try to imagine what is happening to me, from the inside. Apparently, there is no point in having any scans at this stage as mutant cells will probably not show up.
My bike-riding has had to take a back seat during the past couple of months for three reasons:
1. During a walk up Mt Solitary with Matthew (when we both had minor falls) my right upper arm sustained an injury which has made it difficult to stretch the arm out (as when riding my bike). I probably should have had physiotherapy but I think I may have left it too late for that treatment to be effective now. Maybe time will be a great healer! [Time was not a great healer. In 2017 I had a total reverse right shoulder replacement. The operation has been a complete success.] My notes about this walk are at Day Walk to Mt Solitary.
2. My wife had an unexpected stay in hospital for an operation that required her to be cared for at home after her release from hospital, so curtailing any thoughts about trips away that I might have had.
3. My son broke his arm while mountain-bike riding a rough bush trail on Boxing Day and he needed some TLC during a recovery period as he only has a live-in cat for company.
2014 - Bushwalking, Cycling and Bladder Spasms
Update to March 2014
At the end of January 2014 I experienced a urine leakage around the site where the catheter enters my abdomen. In all probability my bladder was over-full and the urine had nowhere else to go. Anyway, at an urgent appointment with the urological surgeon he suggested a slightly larger diameter catheter might fix the problem. I now have a size 22 catheter instead of a size 20 (only a small increase in diameter but enough to stop any leakage). I wonder where this possible repeated increase in catheter size might eventually lead. Do they even make a size 50 catheter?
The next scheduled appointment will be my annual cystoscopy and bladder wash-out during June 2014, to get rid of any accumulated bladder stones.
Update to August 2014
During April 2014 Matthew and I spent 10 days on King Island. We wanted this to be a bike touring holiday but the logistics proved to be too difficult to arrange in the time we had allowed so this was a tour mainly using a vehicle. Trip notes are at Visit to King Island.
My annual cystoscopy and bladder wash-out took place in June, as scheduled, to remove any bladder stones that had formed. On this occasion there was some debris, rather than actual stones. The debris had not caused any problems for me.
The only disappointing development was that my PSA had risen to 16.3. I am not feeling any ill effects of having cancer and so far this is just a number. I know that eventually I will need to have hormone therapy but the longer I can delay the inevitable the happier I will be.
Matthew and I walked from Maydena to the Eagles Eyrie, at the top of Abbotts Lookout on Sunday 18/8/14, after reading about the neglected tourism venture in Hobart's Mercury newspaper. A very stiff walk on a broad, cleared route beneath the power lines. Notes are at Day Walk to Eagles Eyrie.
On 25/8/14 I decided to ride to Sorell and back (41kms) as I had not been riding very much. I think I may have over-stressed my body because, for two days after the ride, I experienced severe bladder spasms and blood in my urine during 25/8. I hope this is not a sign of my body falling apart. It would be a great pity if my bike-riding activities were to be at an end.
Our next walking adventures are a return visit to Maria Island and a few days visiting some of the old huts in the Central Highlands - an area that we have not visited very much to date.
2015 - More Bladder Stones and PSA Increases
Update to March 2015
In September 2014 Matthew and I visited Maria Island again ( Third Visit to Maria Island ). This was a very pleasant trip, where we explored the possible link from Robeys Farm across a direct route to the east coast.
Healthwise, my PSA reading had risen to 16.5 - not a dramatic increase from 16.3 six months previously - but a rise nonetheless.
On our Tasmanian Trail walk in December 2014 ( Walking the Tasmanian Trail - Part 1 ) I experienced severe bladder spasms while in my sleeping bag at night, probably from the extended walking exercise carrying a heavy pack. I did not really have an answer to this, apart from stopping walking.
In the days leading up to my regular four-weekly catheter change in January 2015 I experienced a much reduced urine flow from the Flip-Flo valve and suspected a build-up of deposits along the length of the catheter and in the valve itself. On checking the internet I "discovered" that silicone catheters have a larger internal diameter than the latex catheters I have been using (obviously having thinner walls). I decided to mention this to the urologist at my next appointment and he confirmed that they might help with urine flow. He did mention, however, that they are not as flexible as latex. I decided to give them a try.
A silicone catheter was used at the next catheter change appointment but, within two days, I had it changed to a latex catheter. The reason was that, not being as flexible, it protruded from my abdomen and caused urine leakage around the entry point. I think I must drink more water in order to keep my bladder flushed out and so help to prevent the build-up of deposits. So far it is helping.
Apart from these problems I still manage to lead a reasonably normal life, although I have not ridden my bike for a few months. No excuses but I will just have to start riding again.
Update to July 2015
As charted at the beginning of this saga, my PSA has now risen to 18.8 (as at 1 June 2015). I do not have any ill effects of my cancer as yet but I am sure they will arise as time goes by.
When the bladder washout and suprapubic cystoscopy were done in June 2015 there were some bladder stones but, fortunately, they had not caused me any problems and I had not been aware that they were in my bladder.
During July (at the beginning of the Tour de France actually) I decided to use my exercise bike during all the ad breaks in the live broadcast over the three weeks of the race. I managed to keep a pretty good record of doing it and have continued to use the bike during just about every evening since then. At the same time I have been drinking my two litres of water. I suppose it would be better spread out over the whole day but this is working for me at the present time.
I have tentative plans to try a round Tasmania bike trip, starting during November 2015. This exercise bike routine might help, leading up to more actual bike riding on the local roads as the weather improves. On this occasion I plan to start on an anti-clockwise trip, so avoiding the initial days of continuous uphill slog that I encountered on my previous attempt in October 2012 ( Solo Bike Ride to Wayatinah ).
My next appointment with the urological surgeon is planned for June 2016, when my now annual bladder washout and cystoscopy take place. If my PSA has risen to about 20 by then he expects to start me on hormone therapy. I'm not looking forward to it.
2016 - Bike Ride Around Tasmania
Update to July 2016
This time my planned bike ride around Tasmania did actually occur. Details are at Tony's Tour de Tasmania.
In April 2016 I had two hernias repaired, following the diagnosis of pain in my left groin. Prior to this operation a blood test showed that my PSA had risen to 19.6. Once again, not a dramatic increase but still rising.
I had another PSA test on 27/5/16 that was at 21.0. This test was done prior to having an annual bladder washout and cystoscopy in early June 2016. After the procedure the urological surgeon suggested that I should have a Prostate Specific Membrane Antigen (PSMA) PET scan. This new scan is apparently capable of detecting lower levels of cancer that has spread than more traditional scans. The drawback was that the cost of the scan, $800, would not be covered by Medicare and, therefore, also not by my health benefits fund. I considered it to be too important not to go ahead with the scan and agreed to it. The radioactive source for the scan was Gallium-68 (Ga68).
The result was that, while there was some cancer remaining in the bed of the now-absent prostate gland and in a lymph node, there was no evidence of cancer having spread to my bones. There was, however, "physiological tracer activity" in the lacrimal and salivary glands, larynx, liver, spleen, kidneys and small bowel. [The oncologist I saw later put my mind at rest as I thought the cancer had spread to all those other areas, whereas this description merely stated that the radioactive source had been detected in those areas.]
I asked whether it would be possible to have surgery to remove the offending lymph node and whether immunotherapy might be appropriate to treat my cancer.
The surgeon said that there might be a risk of unacceptable complications with surgery and that lymph nodes are junctions in the whole lymphatic system. He offered to provide a referral to the Melbourne-based surgeon who had performed my radical prostatectomy and who could provide more definitive advice if I wished to follow that course of action. Also, while he stated that he was not aware of any trials or treatment in Australia by immunotherapy for prostate cancer he would provide a referral to a Hobart-based oncologist for a discussion about possibilities in that area.
I have a further appointment with the urological surgeon in January 2017.
In the meantime, I am thinking about a possible bike tour of King Island, either with or without Matthew, depending on his leave situation at the end of 2016.
Update to September 2016
The appointments to review my cancer situation took place at the end of August and in the first week of September. The results were that immunotherapy is not yet available in Australia and the oncologist was not aware of any clinical trials specifically for that form of treatment. The surgeon I saw in Melbourne confirmed that the risks with any further surgery in the area of the prostate bed included the possible loss of my bladder, with the result that I would need a permanent external bag for urine collection and disposal. Obviously, from my point of view, an unacceptable risk, considering that I am able to cope reasonably well with the suprapubic catheter and flip-flo valve to control my urine flow.
He did mention, however, that, given my level of fitness, it might be appropriate to delay starting me on hormone therapy until my PSA reached about 50 or when my PSA level doubled in three or six months. That was a pleasant surprise but reinforced my understanding of current thinking that there is no fixed level of PSA at which to commence hormone therapy.
When I had my PSA checked on 8/9/16 it had risen to 25, up from 21 on 27/5/16. No adverse effects on me at this stage, so life continues as before.
2017 - Riding the Munda Biddi Trail in WA
Update to January 2017
An unexpected complication occurred on 30/11/16 while Matthew and I were riding on the Tasmanian Trail. We had arrived in New Norfolk and booked in to the Junction Motel, near the lower roundabout.
When I was preparing to have my shower at the motel the catheter came out of my body. In a state of shock I quickly pushed the catheter back through the hole in my abdomen into my bladder and securely taped it in position. Normally, the catheter is held inside my bladder by a small balloon that is inflated with 10cc of sterile water at a four-weekly catheter change.
I told Matthew of my predicament so we walked gingerly (at least I did) to the New Norfolk Hospital/Community Health Centre to find a nurse who would be able to do an urgent catheter change for me, using the spare catheter I had with me.
The staff could not have been more helpful, changed the catheter and provided me with some replacement spares in case of another emergency. It was found that the balloon at the end of the catheter had burst and the catheter was not held inside me as a result. I was advised it would be preferable for me not to exert myself too much while riding my bike!
As we left the Community Centre I wondered what would happen if I had another emergency while travelling on Jefferys Track or other bush tracks to Dover.
The blood tests I had on 30/12/16 showed that my PSA has now risen to 30. Obviously, this is going to continue to head upwards, but at the appointment with the urological surgeon on 12/1/17 he seemed to be in no particular hurry to start me on hormone therapy.
I intend to keep on pursuing my bike rides - next on the list is a ride with Matthew, my son, to Smithton via Queenstown and the Western Explorer at the end of this month or early February 2017.
Update to April 2017
Matthew and I rode from Lauderdale to Smithton in the two weeks starting from 31/1/17. (Notes are at Ride from Lauderdale to Smithton.) While riding along the Lyell Highway between Derwent Bridge and Queenstown I experienced a period of extreme stress when my catheter became blocked. This occurred as we were descending Mt Arrowsmith in rain, with nowhere sensible to stop. By the time we reached the information shelter at Franklin River I was barely coherent. Matthew helped me by getting the spare catheter and associated equipment out of my pannier bag. When I was able to release the urine by cutting the tube that held the internal balloon in place in my bladder and withdrawing the old catheter, the feeling of relief was instant.
I believe the reason this situation occurred was because it has not been possible for me to drink sufficient water while riding long distances to adequately flush out my bladder. It is a lesson I need to learn on future rides, otherwise I expect the same situation will occur again.
My next appointment with the urological surgeon is due in June 2017, when I expect him to perform my annual bladder washout to remove any accumulated bladder stones and to check my bladder for any other potential problems. At that appointment he might suggest it is time for me to start hormonal therapy. I suppose it will need to happen sometime.
Update to June 2017
Imagine my surprise when I received the results of my June 2017 PSA test! The reading had gone from 30 in December 2016 to 26 on 2/6/17. The urological surgeon could offer no explanation when I saw him at the bladder washout procedure, except to say it was better than having risen. So that made me feel happy.
There were bladder stones that he was able to remove successfully. The next appointment is for June 2018, unless there are unexpected adverse developments in the meantime.
Update to September 2017
At the end of June 2017 Matthew suggested we should take our bikes, complete with all camping gear, and ride the Munda Biddi Trail, a 1,000kms long off-road MTB track that commenced east of Perth, WA at Mundaring and ended in Albany.
This sounded like an amazing adventure and we prepared to leave in the first week of August 2017. In the intervening time I obtained supplies of Vesicare (with alternatives of Oxytrol patches and Ditropan tablets) to help prevent bladder spasms that had been a problem for me on previous multi-day rides. The Vesicare worked for me and I did not need either of the other drugs. I took with me sufficient spares of catheters and Flip-Flo valves to enable me to have catheters replaced at more frequent intervals than the normal four weeks. My thinking was that, if I had the catheter changed each two weeks, there would not be such a build-up of deposits in the catheter that would result in a blockage. I also arranged to have a normal catheter change the day before we were due to fly to Perth.
During our ride I had a catheter change at Collie Hospital after two weeks and another at Albany during a visit to a local doctor after a further two weeks. At this second catheter change a rather large stone was found to be almost completely blocking the drainage hole at the inner end of the catheter. It was changed not a moment too soon.
Each day of our stay in Western Australia I cleaned the overnight drainage bag using bleach tablets dissolved in water and flushed the fluid through the bag. This ensured that the bag remained relatively clean and free from deposits the entire time we were away. I also made sure I cleaned the catheter entry site in my abdomen and changed the dressing daily.
2018 - Chemotherapy and Androgen Deprivation Therapy
Update to May 2018
My PSA blood test on 29/11/17 showed a rise from 26 to 29. At a subsequent visit to my GP he remarked that my PSA seemed to be stable. I wished I could have been more of a "glass-half-full" person with that news because I doubted if my PSA would maintain that sideways trend.
Early in May 2018 I developed a painful ache on the right side of my back, below the shoulder blade. I thought I had probably strained a muscle while working on the (flat) roof of our house. After 10 days of no improvement I decided, with some encouragement from my wife, to get the ache checked out and I was referred for a CT scan of my chest.
At the GP appointment to review the findings I was somewhat shocked to be told that the pain I was experiencing was probably a result of the spread of my prostate cancer to the area of my ribs at the back and to several thoracic vertebrae. In addition, there were at least eight soft tissue density nodules at various places in both lungs that are probably cancerous. [These were subsequently discovered to be non-cancerous but more likely old scar tissue from a childhood chest infection perhaps.]
Although I was unprepared for the news about the cancer spread, I knew I still had prostate cancer that was not then being treated. Therefore, given time, the cancer was certain to progress in some way. A PSA test on 17/5/18 revealed that my PSA had risen to 74. Another test soon after showed a PSA level of 71.
I have been referred to an oncologist in order to determine what might be the best course of action for me, given that I still want to be able to continue touring Tasmania by bike (planned for November or December 2018). I believe that any further radiotherapy to the pelvic area is not an option for me, given my high dose rate radiotherapy in 2004. My online reading has indicated that maybe a combination of androgen deprivation therapy (ADT) and chemotherapy given together might be appropriate. I may be able to have more radiotherapy if the spread of the cancer is not extensive.
I think a new chapter of my life has begun.
Chemotherapy and Androgen Deprivation Therapy
Update to June 2018
In early June I had my annual bladder washout, after having suffered no adverse events (such as blocked catheters) during the previous year. However, the urological surgeon who performed the procedure must have realised that there was a greater number of stones in my bladder than before. As a result he recommended that I have the next bladder washout after six months, rather than wait for a year to pass.
This image shows just how many stones were extracted from my bladder on 7/6/18. The urological surgeon informed me that some were 2cm overall and needed to be blasted by laser (laser lithotripsy) before they could be removed.
Prior to my visit to the oncologist in mid-June to determine what might be the next phase of my cancer treatment I was booked in for a PSMA PET/CT scan (Prostate Specific Membrane Antigen Positron Emission Tomography/Computed Tomography). Although this scan shows where prostate cancer has spread to, the cost of AUD 600 is not covered by either Medicare or any private health care fund. I paid.
The resulting report and images showed that the cancer had spread to multiple areas, which meant that any further radiation therapy was out of the question.
During discussions with the oncologist the option to have immediate androgen deprivation therapy (ADT), combined with chemotherapy, was suggested. I could have delayed the chemotherapy but, as I want to be able to get fit enough for bike riding later in the year, I agreed to have the full package immediately.
The paperwork that was provided to me included a daunting list of possible side effects from both the hormone therapy and chemotherapy. However, I was informed that it is rare for a man to have many of the problems listed. Time will tell. The ADT consists of 1 x 50mg tablet per day of Cosudex for one month and a three-monthly subcutaneous injection of a capsule of 1 x 10.8mg of Zoladex. The chemotherapy consists of a number of 21-day cycles of Docetaxel drip injections into a vein.
The oncologist arranged some blood tests, including PSA for 22/6/18. When I received the results I was surprised and pleased to see that my PSA had fallen to 53. She explained that this was the effect of the ADT tablets that I had been taking for the previous two weeks.
So far, so good! After the initial doses of drugs on 28/6/18 I have felt surprisingly lively, with none of the potentially serious side effects that I had read about. That is, apart from a slightly flushed face I discovered just before I attended a specialist's appointment for a knee injury.
Update to July 2018
On 1/7/18 I realised I needed more rest than usual so I assumed this was another issue I needed to be aware of.
I had the second of six chemotherapy infusions on 19/7/18 following blood tests that were done on 16/7/18. At the oncologist's appointment she informed me that my PSA had now fallen to 14.2. This was quite a surprise for me - but a very welcome one indeed. I realise that this does not mean I am on the way to a cancer cure but it certainly was better news than if the reading had risen.
There are still no discernible side effects of this treatment that might cause me any problems, which is a great relief. The next blood tests are scheduled for 6/8/18, with the oncologist's appointment on 9/8/18.
Update to 9/8/18
At the appointment with the medical oncologist on 9/8/18, after which I had the third infusion of chemotherapy, the first thing she said to me after asking me to have a seat was: "Your PSA is now at 2.3." My unprepared reply, right from the heart, was: "Holy Shit, is that right?" I then apologised for the outburst. On seeing the result on the pathology report I believed her. I suppose what this means is that the combination of chemotherapy and hormone therapy seems to be having a positive effect, without any severe side effects so far.
With a bit of luck I should finish the sixth, and final, session of chemotherapy on 11/10/18 and I will be between hormone therapy implants (three months apart) when my and Matthew's Northern/Eastern Tasmania bike trip is scheduled for the end of October and through to the middle of November 2018. In the meantime I am using my exercise bike, rowing machine and shortish (up to about 50kms) bike rides to help to keep a bit fitter than I otherwise would be.
It will be interesting to see where my PSA is at the next appointment on 30/8/18. So far, so good!
Update to 30/8/18
Following a series of blood tests done on 27/8/18 I was pleasantly surprised (not shocked this time) to learn that my PSA had further reduced to an all-time low of 1.0. In addition, the reading for ALP (Alkaline phosphatase) had reduced from 143 to a within-range reading of 90. The reference range is 35-110. ALP is an enzyme found in several tissues throughout the body. Elevated levels of ALP in the blood are most commonly caused by liver disease or bone disorders. The medical oncologist explained that, for me, this was an indication of reduced activity of prostate cancer in my bones. Obviously, good news.
So far, I have had minimal side effects from this treatment. The most concerning is that my hands have become very dry, with painful cracks opening up in a dozen places on both hands. I am now using hand cream and rubber gloves more often than I had in the past, in the hope that this issue will clear up quickly.
Update to 20/9/18
The improvements have continued, as reflected in my blood test results from 17/9/18. My PSA level has now reduced to 0.6 and may even go to a lower level in future blood tests. Obviously, I was very happy with that. In addition, the ALP level that I mentioned above has now fallen even further, this time to 72. Apparently, this is further evidence of reduced cancer activity in my bones.
The problem that I was experiencing with cuts on my fingers has now virtually gone, following a determined effort to take better care of my hands.
At the appointment with the medical oncologist on 20/9/18 I explained that my eyes had been watering - if they were tears they would have been tears of joy! - but apparently this is one of the side effects of chemotherapy and should diminish after I have finished that treatment in three weeks time.
Meanwhile I am trying to keep as active as my cancer treatment will allow, including the occasional 40 - 50kms bike ride and daily walks to buy the morning paper. My weight has increased from normal, which was between 81 and 82kgs to nearly 85kgs. Not dramatic but something I will need to be careful about. Maybe I am eating more but the treatment probably plays a part in the increase.
Update to 11/10/18
At my appointment with the medical oncologist on 11/10/18 I learnt that my PSA had reduced to 0.42 - a very encouraging result. Also, the ALP level (please see description above) had dropped from 72 at the previous appointment to 66. The acceptable range for this is between 35 and 110. The current reading is a dramatic improvement from a highest level of 244 on 22/6/18. I must admit I don't really know much about this but if the number keeps reducing I think I will remain happy about it.
I have now finished the course of six three-weekly chemotherapy infusions and will now continue on with the three-monthly pellet implants of the hormone treatment. So far I feel OK, especially considering that I could have been suffering from multiple side effects during the past 18 weeks.
It is now my intention to concentrate on Matthew's and my upcoming bike tour of Northern and Eastern Tasmania, starting from Smithton on 26/10/18. I am approaching this with some mild trepidation as I have not been able to devote as much time to riding and improving my fitness as I would have wanted to. However, our philosophy is that we will try to ease into the riding task and improve our fitness as we go.
Androgen Deprivation Therapy (continuing)
Update to 13/12/18
Since my previous update our bike ride has actually happened. Notes on this trip are still being prepared but in time I will link to the report. [Notes are now at Bike Tour North & East Tasmania.] Very tough going for me, although Matthew seemed to take it all in his stride and showed great patience with my slower pace throughout the 14 days we were riding. No issues with my SPC but I arranged to have the catheter changed at St Helens Hospital as a precaution while we were there on a rest day, specifically for that purpose.
I have recently had two PSA blood tests; results were 0.17 on 26/11/18 and 0.14 on 10/12/18. I am very encouraged by these very low readings and hope that the ADT drugs are having some positive effects.
The first blood test was in preparation for a bladder washout on 7/12/18, at which the urological surgeon apparently found no bladder stones, only some debris. As a result he has scheduled the next appointment for one year rather than in the next six months.
The second blood test was done a few days prior to my appointment with the medical oncologist. She was pleased with this result and said that I seemed to be coping very well with the ongoing hormone therapy. After this appointment a new pellet implant was inserted into my abdomen - an ongoing three-monthly procedure.
2019 - PSA Nearly Zero and Low Testosterone
Update to 7/3/19
The good news continues. My PSA reading for 1/3/19 was 0.08. I wonder for how long this encouraging downward trend will continue. I think that, when the PSA starts to rise again, I will probably be on another round of chemo.
The oncologist was very happy with that result and pleased that I am not suffering from the effects of having the three-monthly implants of ADT (Zoladex).
Matthew and I are now thinking about a possible visit to New Zealand later in the year, with our bikes, to ride some of the trails on the South Island. The GP who I mentioned it to has asked me to provide him with a rough route itinerary in order that he is able to provide a letter to an insurer for travel insurance purposes. Logistics are still to be worked out.
My next appointment for another ADT implant is at the end of May 2019.
Update to 26/8/19
Well, I missed the update for May. However, there really was not a great deal to report. My PSA has continued to be very low (around 0.1 to 0.08). I, and more importantly, the medical oncologist remain optimistic that, for the time being, my cancer seems to be under control. I do not have any significant side effects from the 3-monthly injections of a pellet of Zoladex that controls my testosterone (also at a very low level <0.1).
I decided that I am not too confident about making the November/December visit to New Zealand a bike tour. Therefore, instead of taking our bikes we will hire a car while visiting the North Island then get a bus and ferry to the South Island to continue with another car trip. I must admit that I felt a bit sad about not making the trip a bike tour. However, we might hire bikes for shorter tours while on holiday.
On 3/9/19 I am due to have another bladder washout and cystoscopy. This has been brought forward from the December 2018 plan to have this done in December 2019 because I have been experiencing a partially blocked catheter that has led to my needing to have more frequent catheter changes (two weeks instead of four weeks between changes).
Update to 3/9/19
After the bladder washout and cystoscopy, done under general anaesthetic as normal, I attended a post-operation appointment with the urological surgeon. He explained that there were many bladder stones in my bladder, some as large as 10mm across. He also expressed some pleasure at my satisfactory progress and stated that he thought I was his fittest patient. Whilst this gave me some comfort I really would have preferred to be his fittest non-patient without prostate cancer! However, I still try to be a glass-half-full person and I suppose this must help me.
Things now seem to be back to "normal" and I should revert to four-weekly catheter changes and another appointment for the next bladder washout/cystoscopy in September 2020.
I will continue to post updates to this account as and when they occur. If you have made it through this far, congratulations on your patience with my commentary.
2020 - Abiraterone Commenced and Point-to-Pinnacle Walk
Update to 11/2/20
My hope that I would be able to have my catheter changes every four weeks did not eventuate. In fact, there have been a couple of occasions when I needed to have a change done after two weeks. In particular, in New Zealand I needed a catheter change after two weeks. Fortunately, I was in Christchurch at the time and I was able to have the procedure done, albeit reluctantly, by a doctor at an after-hours clinic. As a result, I will be having another bladder washout and cystoscopy sometime in March 2020, date not yet fixed.
Although it is not obvious from my chart at the beginning of this account, my PSA has now risen to 0.24, from 0.10 in August 2019. When I saw the medical oncologist on 6/2/20 she pointed out that my PSA, while still very low, had doubled in six months. This, apparently, was a trigger for further intervention to occur.
The immediate result is that I am about to start a course of monthly injections by my GP of Denosumab (Xgeva). This is a drug that has been shown to reduce progression and complications from prostate cancer in the bones.
In addition, I may be eligible to participate in a clinical trial called "A Phase 3 randomized study of Niraparib in combination with Abiraterone Acetate (Zytiga) and Prednisolone for treatment of metastatic prostate cancer".
A blood test to be taken in the next two or three weeks will determine if I can take part or not. I will post further details when I know if I will be included in the clinical trial or not.
Update to 20/3/20
A blood test done on 24/2/20 showed that my PSA had risen, marginally, to 0.27. Still very low but rising nonetheless.
The bladder washout could not wait until September 2020 as I was experiencing a much reduced urine flow through the catheter during February. A procedure was scheduled for 3/3/20. After the bladder washout and cystoscopy the urological surgeon showed me the single stone that had been removed from my bladder. It measured about 5mm across - not huge but large enough to block the end of a catheter at some time. The next procedure is scheduled for 12 months down the track. It remains to be seen whether or not I am able to cope until then.
On 18/3/20, at an appointment with the medical oncologist, I signed the consent form to have preliminary tests performed in readiness for being considered for the clinical trial mentioned above. The first test was to take a blood sample that would be analysed to determine if there was a gene mutation present. If not then I would not be considered for the trial. The second test is to be conducted on a prostate tissue sample that had been taken a few years earlier. Results are still awaited at this time.
In the meantime I have commenced a course of Abiraterone Acetate (Zytiga) with Prednisolone, regardless of whether or not I will participate in the clinical trial.
In general, my health is still reasonably OK. However, my weight is now around 84.5kgs, despite some bike rides and some care being taken over what I eat.
Update to 14/4/20
Well, the results are in! Apparently, the blood and tissue samples revealed that I do not have the necessary gene mutations that would make me eligible to take part in the study (Study 64091742PCR3001). In a way I was relieved to get that result as the clinical trial would have involved an initial 3-years on Niraparib with frequent scans and hospital appointments, plus up to an extra 5-years post-trial study. It would have been an arduous experience, especially as this is a double-blind trial (meaning that 50% of the participants are given a placebo instead of the drug being trialled and neither the researchers nor the patients know which group the patients are in).
The other positive from my recent blood tests is that my PSA has now dropped to 0.07. As I am currently experiencing no serious side-effects from the new treatment I am encouraged by this result.
Update to 11/5/20
The latest PSA reading is now at 0.04. Clearly, this is as a result of my taking Zytiga. Fortunately, the side-effects for me are minimal - hot flushes from time to time. Those I can live with.
The next appointment with the medical oncologist is due mid-June. So far, so good.
Update to 20/7/20
As shown on the charts at the beginning of this saga, my PSA has now reached a level at which it is said to be <0.03. The medical oncologist said this means the PSA is undetectable. For the sake of producing charts I have assumed a level of 0.02. Either way, I am encouraged by the last two results.
On a recent bike ride to South Arm, Tasmania, with my son I found I was struggling on hills that in earlier times I would have managed relatively easily. Do I put this down to the effects of the hormone therapy reducing my strength levels, or - more likely - the effects of old age?
I am still planning to do longer, multi-day rides towards the end of 2020 when the COVID-19 pandemic might be a little more under control. This remains to be seen.
In the meantime, I still enjoy getting out on long walks and reasonable length (50kms) bike rides.
Update to 29/10/20
My PSA continues to track at a very low level - still <0.03. I don't know how long this low result will last because I believe the cancer will once again rear its ugly head and counteract the positive effects of my treatment. I intent to enjoy life as it presents itself here and now and not concentrate on what might or might not happen in the future.
During the past six weeks, since the first week in September, we were lucky enough to have adopted a rescue dog from an animal sanctuary in North-East Tasmania. She is a 2-year-old cross between a Shih-Tzu and a Blue Heeler (a Blue-Tzu-Heeler). A delightful dog but, as we are reluctant to leave her at home by herself, my bike rides and walks have been somewhat curtailed. That is a small price to pay for the privilege of having another dog after we had to end the life of our previous dog, Flossi, in August 2020. I wrote a tribute to this beautiful pet that can be found at 228 Days With Flossi.
My next physical challenge is to complete the 21.5kms Point to Pinnacle walk on 16/11/20. I previously did this walk in 2012. This will be a significant challenge, being predominantly an uphill slog up Mount Wellington to the summit.
Update to 13/12/20
After having done some preparatory walks; from the Casino to Fern Tree and return (20kms); from Fern Tree to the Pinnacle and return (24kms); I felt ready to tackle the entire walk from the Casino to the Pinnacle on Monday 16/11/20. Matthew was a great help in providing drinks, snacks and plenty of encouragement while I plodded for 4hrs 42mins in, at times, torrential rain and pleasant sunshine.
This was part of a Strava Challenge, the real Point to Pinnacle having been cancelled due to you-know-what.
As can be seen from the chart at the beginning of this account, my PSA continues to be undetectable and my other blood test results are not causing the medical oncologist any concern.
On 30/11/20 I had a cystoscopy and bladder washout as I had been experiencing a very slow urine flow through the SPC after a very short time since a previous catheter change. The urological surgeon who operated told me that he removed 10 large stones and 20 small stones. He remarked that it was no wonder that I had been experiencing problems with urine flow. Next appointment is scheduled for December 2021, unless I have problems at an earlier date.
My next challenge is to start back on my bike - not having ridden since early September will be a challenge in itself but one that I want to achieve.
Our new dog continues to enthrall and entertain us. She is a beautiful addition to our family.
2021 - PSA Undetectable and More Bike Rides
Update to 4/1/21
The latest blood test indicated my PSA was still undetectable (officially <0.03). Naturally, this is very encouraging and I will continue to be pleased with the low rate, as long as it lasts.
My bike riding has resumed, with several local day rides of between 35 and 70kms. It has taken a bit more effort than I remember I used to need to exert but that can probably be attributed to a combination of old age, a combination of anti-cancer drugs I am taking and a lack of recent riding. I can do something about the latter problem but no serious plans for long-distance, multi-day rides at this stage.
Update to 16/5/21
So, it's business as usual! My PSA continues to track at a very low level - <0.03 when blood tests were taken on 10/5/21. The medical oncologist was very pleased with this result, and with all the other blood test results from tests taken at the same time.
I have been trying to get out on my bike more frequently than previously and have ridden distances from 35kms to 96kms during the past few months and some long day walks, up to 35kms in length.
My weight has now stabilised around the 80kgs to 81kgs level but I am working on reducing it to the mid-70kgs.
Now that the Giro d'Italia is in progress I have been watching every stage live and using my exercise bike in the ad breaks. I hope to continue this through the Tour de France and the Vuelta a España later in the year. Obviously, the exercise bike is a poor substitute for a real ride but the weather tends to dissuade me a bit.
Update to 24/11/21
Nothing unusual to report as far as my PSA is concerned - still undetectable at <0.03. Good news.
On a short, easy bushwalk with Matthew and Candy in mid-May I had a fall while clambering over a fallen tree trunk and eventually needed to have a serious right lower leg wound debrided that had become infected. See trip notes at Day Walk to Brown Mountain 15/5/21.
After the operation, that necessitated an overnight stay in hospital, for the next four months I attended a local clinic to have the dressing changed until the wound had healed. I must be getting clumsy in my old age!
On 9/11/21 I attended hospital for an annual catheter cystoscopy and bladder washout. The urological surgeon who performed the procedure told me that there were several small stones, that he removed. I had not been having any blockages or other adverse events so the next scheduled procedure will be in December 2022.
During October I signed up for the Great Cycle Challenge. This was to aid research into eliminating cancer in children. I nominated a distance of 500kms and amount of $500 that I thought I could achieve during the month.
As the days progressed, thanks to generous donations from family and friends, I was able to gradually increase my goal to $1,800 - which I attained with a few days to spare before the end of October. I also achieved the distance goal of 500kms. The distance goal was not made any easier when a 3-day lockdown was imposed on Southern Tasmania and exercise was restricted to a 5-kms radius of home. I still managed to average around 45kms by riding laps of my local roads, even though it was somewhat monotonous.
For my efforts I was presented with a bike-riding shirt, a handsome medal and a certificate.
2022 - PSA Still Undetectable and More Bike Rides and Walks
Update to 28/1/22
Pleased to note that my PSA is still undetectable (<0.03) - as shown in the graphs at the beginning of this account. Testosterone level was <0.2. Other blood test results were all satisfactory.
I have continued to ride about once a week with distances around 40-50kms. My favourite destinations are coffee shops in Sorell or Richmond or South Arm. There are no plans in place for any multi-day rides but maybe they will happen next summer.
I also walked 35kms from home to Seven Mile Beach, then to Five Mile Beach and back home in early February.
Update to 23/5/22
Not much to report at this stage, except my PSA has continued to be undetectable, and my bike rides and walks continue to give me a great amount of pleasure. Rides have been to Richmond, South Arm, Dodges Ferry and Sorell.
I think my days of long-distance bike rides and overnight bushwalks might have come to an end. Maybe the effects of androgen deprivation therapy, combined with old age, mean that my core strength has weakened, despite my efforts to undertake whatever exercise I am able to. However, I still feel healthy so I will continue to ride and walk whenever I can.
Update to 21/12/22
I continued my rides, as noted above, leading up to the beginning of October, when my participation in the Great Cycle Challenge 2022 began. I had set myself the targets of raising $500 towards the elimination of cancer in children and riding 500kms during October.
As at 31/10/22 I had exceeded my riding goal by riding 551kms in 13 rides and managed to raise $2,095, thanks to generous donations from relatives and neighbours. However, on 3/10/22, while riding from west to east on the Tasman Bridge, my right handlebar clipped the steel mesh barrier of the narrow path and flipped me off my bike onto the concrete path. Some injuries to my right eye socket, right arm and left knee and ankle. I was probably going a bit faster than the 15kms/hr speed limit and was not concentrating enough. After checking for broken bones I rode the remaining 17kms back home. No real damage to my bike except I needed to straighten the handlebars back to the correct position before restarting.
Overall, I was happy with this effort.
Blood test results on 4/11/22 showed my PSA still undetectable (as per charts at the start of this account) and other results within range.
On 20/11/22 I will walk the Point to Pinnacle 22kms (not a race for me) and in the meantime I will need to make a determined effort to walk more challenging distances than just along the beach with our dog Candy. I am looking forward to this challenge.
The Point to Pinnacle happened, finishing the walk in 4hrs 32mins 8secs, just 8mins ahead of the 4hrs 40mins cutoff time!
The following timeline details issues I had with my catheter around Christmas-time 2022.
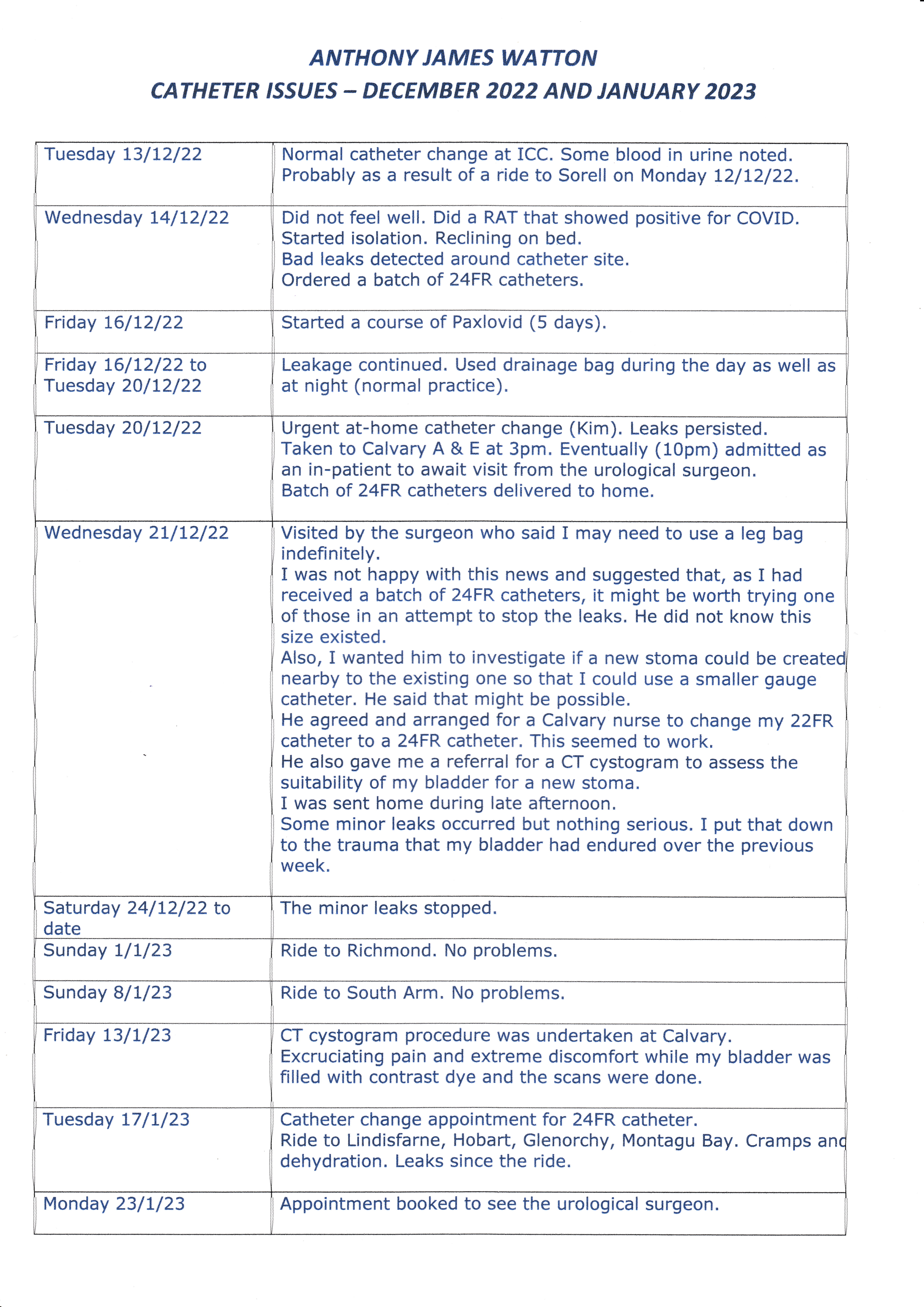
2023 - Bike Rides, Catheter Leaks and a New SPC Site
Update to 25/2/23
As can be seen in the chart at the start, my PSA has risen, marginally, to 0.04. The medical oncologist considered that this could be explained by the traumas that my bladder area had experienced over the past two months. It will be interesting to see the result at the next blood tests in three months time.
At the appointment with the urological surgeon on 23/1/23 I mentioned that the 24FR catheter was still leaking at the SPC site. I asked him if it would be possible for me to have a second SPC site, close to the existing one, with a much smaller diameter catheter. My thinking was that, over time, the new hole would slowly enlarge - just as the old one had - and there would be sufficient leeway for a larger catheter over time. He agreed and wrote a referral for a new SPC site to be cut under CT cystogram guidance.
This procedure was carried out on 31/1/23 under local anaesthetic and a new size 14FR catheter was inserted. Over the following three weeks there was no urine leakage and the old SPC hole appeared to be sealing satisfactorily, with no sutures or other closing aids.
During this time I wore a urine collection leg bag during the daytime and my normal drainage bag overnight in order to avoid a build-up of pressure within my bladder that might contribute to urine leakage. I think this will prove to have been a good decision and now I am impatient to start riding my bike again. At that time I intend to switch from using a leg bag to a flip-flo valve to control urine flow.
Meanwhile, the urological surgeon wrote to the Continence Clinic stating that he wanted me to transfer, over the next three months, up to a size 20FR catheter. I was not happy with this development and, after discussing this with the Continence Clinic nurse, it was agreed that at the next catheter change on 28/2/23 I would go up to a size 16FR catheter and stay at that size for the foreseeable future. I can understand his concern as I have had a history (not recent however) of bladder stones that blocked the end of the catheter.
Update to 11/5/23
So far, so good with the size 16FR catheter. After an initial settling-down period I am satisfied that I made the correct decision to have a relocated SPC site and a smaller catheter.
Not all roses, however. At my most recent appointment with the medical oncologist she told me that my PSA has now risen to 0.07. She explained to me that, having been on this particular cancer treatment for over four years, some of the cancer cells have mutated and are now resistant to my medication. If my PSA continues to rise to, say 0.2, I may need to be on a different medication or have another (different) course of chemotherapy.
In the meantime I have resolved to get out on my bike at more regular intervals and do some reasonably long walks in an effort to raise my level of physical fitness. It may or may not work.
Update to 8/12/23
My PSA has continued to rise and, as at 29/10/23, is 0.16. That might not sound significant but the fact remains that my cancer is still active somewhere in my body.
The medical oncologist does not want to prescribe another PSMA PET scan just yet as she considers that no cancer cells will be able to be detected at this low PSA level.
All that aside - as in 2021 and 2022 I signed up to ride in the Great Cycle Challenge during October. However, those plans took a severe beating because, on 17/9/23 I came off my bike at low speed. The huge haematoma that immediately formed on the inside of my right knee required draining and on 29/10/23 I came off my bike again, this time injuring my left knee. Fortunately, this injury did not need medical intervention but a fair amount of R & R.
My achievements for kilometres ridden and dollars raised were: 542kms and $1,519. I was happy with that result but I hope to do better next year, hopefully without the accident dramas.
During November Matthew and I travelled to Victoria, taking Matthew's car on the ferry, to ride the Great Victorian Rail Trail from Mansfield to Tallarook. As we had a vehicle we were able to ride out-and-back legs of the trail then take the car to the next intermediate destination. This enabled us to ride the trail in both directions by the time we reached Tallarook. Total distance ridden was 280kms over 6 days. A great experience.
2024 - More Bike Rides, Walks and Rising PSA
Update to 25/1/24
It came as no surprise, but with some disappointment, that at my appointment on 25/1/24 the medical oncologist informed me that my PSA has now risen to 0.18. While this result is still very low it means that some additional intervention may be appropriate in the not-too-distant future.
With the expectation that my PSA will have risen to 0.2 within the next three months a PSMA PET scan will be done in April 2024, just prior to my next appointment with the medical oncologist.
If the scan shows that there are isolated cancer spots then these may be able to be treated with radiation therapy. If, on the other hand, the cancer spread is more general then a course of chemotherapy may be more appropriate. I'll just deal with whatever comes along.
More concerning news is that the urological surgeon who has overseen my catheter/bladder issues for the past 15 years has decided to retire. No contact has as yet been made with an alternative surgeon but it is essential that I continue to have professional oversight of the various potential problems that my SPC may throw up at me.
Long walks (around 20kms) are continuing, as are my bike rides of between 45 and 60kms.
Update to 5/6/24
As planned, the PSMA PET scan was done in April, with no remarkable, abnormal issues to report. This does not mean that my cancer has miraculously disappeared, rather that the spread cannot at present be detected. So I suppose that is good news.
Also, during April, I was referred for an X-ray of my left jaw. I had experienced some pain in that area and had become concerned about the possibility of disintegration of my jaw, due to the Xgeva injections every 3 months. Fortunately, the X-ray was negative for any abnormality. Am I being paranoiac?
I have managed to find another urologist and another GP for my continued care. All good so far.
Oh, and my PSA has now risen to 0.25, up from 0.18 three months previously. Possible further treatment at some time in the future includes targeted radiotherapy and/or a different form of chemotherapy.
I continue to ride distances of between 40kms and 70kms and walk between 12kms and 20kms. I hope the exercise is helping me.
Update to 7/9/24
I wasn't surprised by the latest PSA result of 0.37 at my visit to the medical oncologist in August. So, even though that is an increase, I have no indication that there is anything adverse happening to my body.
My new GP had noticed that, on the PSMA PET scan report, I have some mild calcification of my coronary arteries. On 6/9 I had a scan of my heart in order to determine if there is anything sinister that I might need to address.
However, I have still managed rides of between 40 and 50kms with no obvious adverse indications. It will be interesting to discover whether I might need to change my habits when I see my GP at the end of September.
In the meantime, I have signed up for this October's Great Cycle Challenge (4th year of participation) with the aim to raise $1,000 and ride 500kms in the month. Also, I have entered the Point to Pinnacle walk that takes place in November.
Update to 15/11/24
As a result of the heart scan my GP has recommended that I start using Rosuvastatin as, as well as the calcification of my coronary arteries, my LDL cholestoral is slightly raised. To be reviewed mid-December.
My plans for the Great Cycle Challenge seemed to be in jeopardy following a left shoulder injury, caused by lifting a full LPG cylinder out of the boot of my car only one week before the start of October. I then planned to ride 100kms instead of my usual 500kms. My plans for fund-raising were still at $1,000.
As October progressed I discovered I was still able to ride and I raised my riding goal to 500kms and fund-raising to $2,000. I was eventually able to ride 632kms and raise $2,316 for this worthwhile cause.
I am now "looking forward" to participating in the Point to Pinnacle, walking, on Sunday 17/11/24. It won't be easy!
Having not done as much hill walking in time or effort as I should have, I struggled up Mt Wellington in a not-very-impressive 4hrs 49mins 58secs. The consolation for me was that I was first in the male 80-84 age group, even though I was the only walker in that group! My son Matthew said, "What about all the other 80-year-old men in Tasmania who didn't even do the walk"
Oh, by the way, my PSA has now risen to 0.39. No evidence as to where the cancer is.
2025 - Bike Rides, Lack of Strength, Rising PSA, SAMRT Radiation
Update to 5/2/25
At my most recent appointment with the medical oncologist I saw that my PSA had risen to 0.54. While this is still a very low level there is only one direction this will go to in future.
I am now resigned to the fact that my cancer drugs are robbing me of my strength. This, combined with old age, is now preventing me from thinking about multi-day bike rides or bushwalks. However, I am still able to ride about 50-60kms and walk up to 20kms so I suppose things aren't too bad for me just now.
Update to 20/4/25
I'm about to enter a new phase in my efforts to stay alive and continue doing things I love to do.
Earlier this month, 9/4/25 to be exact, I had another PSMA PET scan. The medical oncologist recommended this because my PSA has now risen to 0.95. Although this level might seem low enough to ignore, the fact remains that the level has more than doubled in a 10-months period.
Somewhat surprisingly, to me at least, the result of the scan showed an "intensely PSMA avid 9mmx8mmx10mm sclerotic metastasis in the left side of the sacrum consistent with a prostate carcinoma metastasis, not evident on the previous PSMA PET scan".
As a result of this development, I have been referred to a radiation oncologist with a view to having a course (maybe up to five sessionss) of stereotactic ablative body radiation treatment (SABRT).
Apparently, this is a highly accurate, multi-directional xray treatment that may eliminate that particular area of cancer. I hope this is correct as I don't wish to have a repeat of my initial HDR brachytherapy in 2004 that eventually left me with a non-functioning urethra.
The initial appointment is scheduled for 2/5/25.
Another worrying observation made in the PSMA PET scan notes was that there is a large hiatus hernia present. In the PSMA PET scan that was done in April 2024 the observation was that there was a moderate size hiatus hernia. Does that mean the hernia has grown in size over the past year? If so, is there a case to be made for an operation to correct the hernia, with possible unpleasant side effects?
Update to 25/6/25
On 21/5/25 I had the first of five SABRT sessions, the last taking place on 30/5/25.
This treatment was painless although I have since exerienced a dull ache at my left hip. Nothing serious.
The painful part was that, even with substantial Medicare funding, I was left out of pocket $2,000 that, fortunately, I was able to cope with.
On 24/6/25 I had an appointment with a gastro-enterologist to discuss possible solutions for my large hiatus hernia. He explained that the hernia had actually not grown since the scan in April 2024, which was quite a relief to me. Therefore, he did not recommend an operation, rather another medication to assist in controlling gastric reflux. It remains to be seen whether this provides a solution to my problem. This was famotidine, that appears to be some help to me.
Update to 15/12/25
Blood test results for September indicated that my PSA had risen from 0.98 at the end of June to 1.20. This was a bit disappointing as I had expected my PSA to have dropped a bit following the radiation treatment in May.
Once again, I signed up to participate in the Great Cycle Challenge. This was my fifth year of the Challenge, attempting to ride 500kms and raise $1,000 in October to help eliminate cancer in children. By the end of October I had ridden 519kms and, thanks to friends and relatives, had raised $2,151 for this worthwhile cause.
At my appointment with the medical oncologist on 13/12/25 blood test results showed my PSA was 1.60, up from 1.20 in September. Although I don't feel ill, I know there are still cancer cells in my body.
It continues to be a great comfort to have the love and understanding of my wife, Suzanne, and my son, Matthew.
I hope that the above might assist other men when considering their options, or at least help to make them and their loved ones better informed about some of the possible issues they may encounter on their journey. Needless to say, there have been significant advances in the treatment of prostate cancer over the past 21+ years. Some, or all, of my experiences and choices may now not be relevant or appropriate when men consider their options.
If anybody is interested in following up with me any questions or comments I can be contacted at nospamtonywatton180@gmail.com. Obviously, the nospam part will need to be deleted to send an email to me.